Rural health reform doesn’t happen in one bill or budget cycle. Success requires people and systems to continuously align how they work, deliver care and manage risk within rural realities. Employers, insurers, providers and policymakers must move together with clear rules and incentives that reflect how rural communities actually function.
Manufacturing and food processing anchor many rural economies. On the floor of a rural Alabama factory, a line worker pauses to stretch a sore shoulder while the shift continues. Down the road, a poultry crew finishes another long day. Workers often ignore small strains and stressors until injuries or behavioral health challenges pull them off the job and into a care system already under strain and short on capacity.
This issue goes beyond health; it involves keeping rural Alabama working.
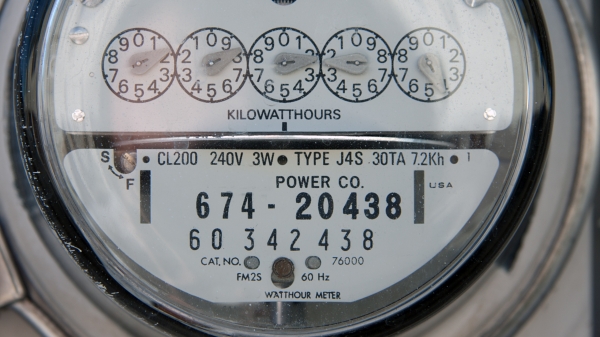
For many rural counties, maintaining worker health proves as essential as maintaining roads or electricity. Local flexibility and coordination often determine access to care. When workers miss routine care, downtime increases, costs rise, and the local economy feels the ripple effects.
Manufacturing and food processing clearly illustrate these stakes. When workers miss shifts, production slows and insurance premiums rise. When clinics fall behind, conditions worsen before treatment. What starts as a manageable problem escalates into a threat to workforce stability, clinic viability and community resilience.
Many local employers keep clinics and hospitals open by keeping workers healthy. Yet small businesses often cannot adjust schedules or offer paid leave for recovery. Insurers struggle to promote preventive care when providers remain scarce, and telehealth depends on broadband infrastructure that remains inconsistent across rural Alabama.
The Alabama Rural Health Transformation Program provides a timely framework to address these pressures. Practical implementation must fit local realities for success. Incentives and rules must reflect rural constraints such as staffing shortages, limited clinic hours, long travel distances and low patient volumes. Alignment only works when each part of the system supports the others.
That alignment looks like this:
- Employers coordinate schedules and maintain coverage where possible, helping workers access timely care without sacrificing production.
- Insurers encourage preventive visits and predictable recovery, but payment design alone cannot overcome provider shortages or broadband gaps.
- Providers adapt care delivery to irregular hours and long distances, yet staffing shortages remain a hard limit.
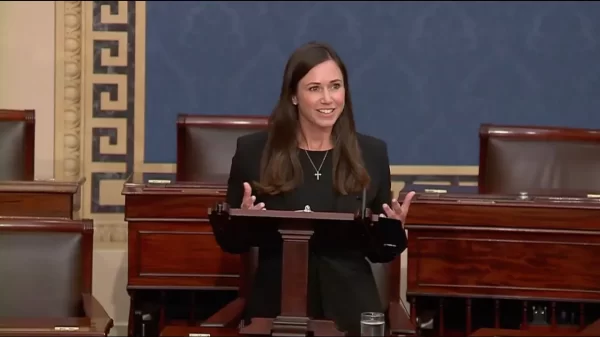
- Policymakers set clear, predictable rules that allow flexibility and recognize rural capacity limits.
- All partners invest in workforce development so communities have enough trained clinicians to respond early, before problems escalate.
Many rural clinics still operate on outdated assumptions. Fixed office hours do not align with shift work, and long travel times put care out of reach for many workers. As patients postpone care, costs rise later. Telehealth can help bridge distance and time, but only where broadband access, clinical supervision and sustainable funding exist.
Behavioral health needs highlight these gaps even more. Stress, chronic pain, anxiety, depression and addiction sideline workers, strain families and place additional pressure on already stretched systems.
Keeping jobs, people and care connected requires coordination, adequate staffing and accessible care pathways. When one-part falters, absences climb, premiums rise and clinics struggle. When alignment holds, recovery improves, turnover stabilizes, clinics gain steady volume and communities strengthen.
Consider a familiar scenario: a small parts manufacturer works with a nearby clinic to treat injured workers around shift changes. Recovery improves, claims stabilize and turnover eases. The clinic gains steady patient volume and grows capacity. No new mandates require action. Alignment simply does the work.
Progress rests on clear expectations and steady signals. When rules and incentives remain realistic, employers invest, insurers innovate and providers expand capacity confidently. When rules appear unclear or misaligned, hesitation spreads and opportunities slip away.
Alabama already has committed employers, engaged providers and insurers focused on long-term stability. But resource limitations, staffing shortages and infrastructure gaps remain unavoidable.
The open question is whether policy reinforces these connections or lets them fray. When leaders across sectors move together and adapt to local constraints, workforce health strengthens local economies, clinics stay viable and rural communities gain staying power.
A healthy workforce keeps rural Alabama working. Rural communities keep health care alive.