Whether Alabama’s health care system will be able to handle the coronavirus pandemic will depend on its people.
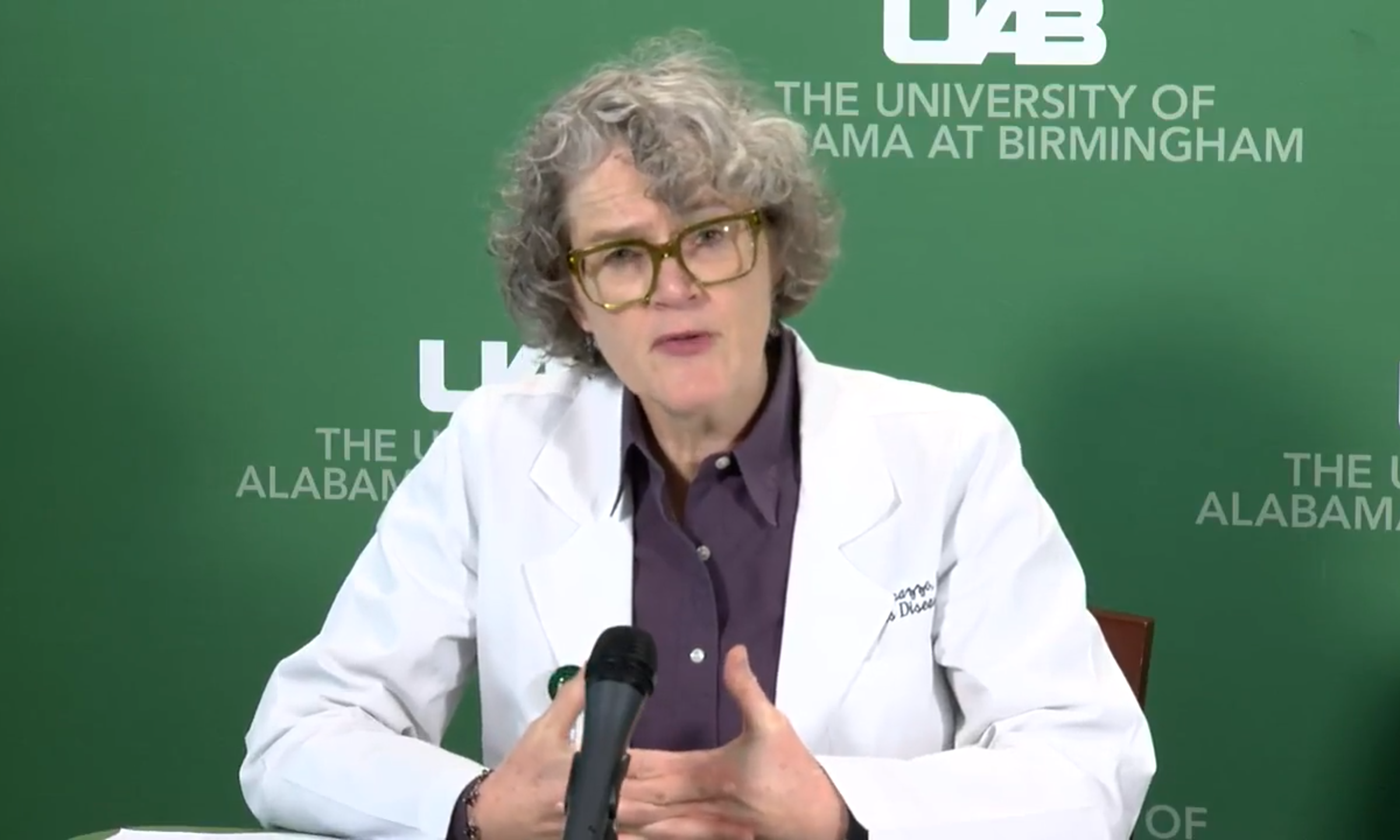
The infectious disease specialist leading the UAB Medicine’s response to the coronavirus outbreak urged Alabamians to take social-distancing measures seriously to blunt the exponential growth of coronavirus cases in the state so as to not overload health care facilities.
An unmitigated spread of the virus—not to be alarmest—could cripple Alabama’s hospitals and leave doctors and other medical workers in horrible situations. Blunting the number of new cases in the near term by limiting social interaction and practicing good hygiene is the only way to prevent a health care crisis, experts warn.
On a call with reporters Monday, Dr. Jeanne Marrazzo from UAB said the closure of rural hospitals, the growth in the number of cases in the state and the potential for a ventilator or ICU bed shortage if the growth curve of COVID-19 cases isn’t blunted is “frightening.”
“In Italy, they don’t have enough,” Marrazzo said. “They are actually having to make decisions about taking people they believe are not going to survive off ventilators to reassign them to people. We do not want to be placed in that excruciating situation. It’s about the worst possible thing I can imagine as a physician, talking to a family about that or dealing with that. I don’t believe there’s any indication we’re going to get there. But again, my assurance is all based on my belief that we can deflect this curve and not be where Italy is right now.”
[visual-link-preview encoded=”eyJ0eXBlIjoiaW50ZXJuYWwiLCJwb3N0Ijo4MzY4MywicG9zdF9sYWJlbCI6IlBhZ2UgODM2ODMgLSBUaGVzZSBjaGFydHMgc2hvdyBob3cgQWxhYmFtYSdzIGhvc3BpdGFscyBjb3VsZCBiZSBvdmVyd2hlbG1lZCIsInVybCI6IiIsImltYWdlX2lkIjo4MzIwMCwiaW1hZ2VfdXJsIjoiaHR0cHM6Ly93d3cuYWxyZXBvcnRlci5jb20vd3AtY29udGVudC91cGxvYWRzLzIwMjAvMDMvQWRvYmVTdG9ja18xODk2ODExNzEtc2NhbGVkLWUxNTg0MjM4NzQ5MzUwLTEwMDB4NjAwLmpwZWciLCJ0aXRsZSI6IlRoZXNlIGNoYXJ0cyBzaG93IGhvdyBBbGFiYW1hJ3MgaG9zcGl0YWxzIGNvdWxkIGJlIG92ZXJ3aGVsbWVkIiwic3VtbWFyeSI6IkhvdyBwcmVwYXJlZCBhcmUgQWxhYmFtYSdzIGhvc3BpdGFscyBmb3IgdGhpcyBmaWdodD8gV2UgaGF2ZSB0aGUgbnVtYmVycy4iLCJ0ZW1wbGF0ZSI6InVzZV9kZWZhdWx0X2Zyb21fc2V0dGluZ3MifQ==”]
Marrazzo said UAB has about 300 ventilators ready for use, which should be enough if the number of cases is limited through social-distancing measures.
But there remains a larger question about the state, and whether the state as a whole has enough ventilators and ICU beds to deal with the COVID-19 epidemic.
“We well know that many rural hospitals have been closing, right,” Marrazzo said. “We’ve been losing a lot of our smaller hospitals. Even those that have remained open may not have a deep staff to take care of critically ill patients. That’s when things do get frightening, and you do need to think about expanding your capacity at a place like UAB or a central place. We have contingency plans that we have been discussing. So this is basic disaster preparedness that people are actively pursuing. But I want to reassure people, we’re definitely not there. And we will be keeping very close, close track of this and updating you all as it comes on.”
Earlier Monday, Alabama Department of Public Health state health officer Scott Harris and Emergency Management Agency director Bill Hastings urged the state to take extra precautions to avoid spreading the disease any further.
“This is a human disease that is going to require a human response, which is going to require a whole of government response, which will require a whole of society response,” Hastings said. “A mobilization of all Alabamians, all U.S. citizens to reduce and slow the transmission of COVID-19. So it stays at or below or around the max capacity of our health care system. That is the fight that we’re in right now.”
The Department of Public Health is monitoring the total number of intensive care beds available and ventilators available for use in the state. Hospitals are required to report their numbers to the ADPH daily—sometimes more often. That number is not publicly available, but some estimates have placed the ICU bed capacity in Alabama’s hospitals at between 1,000 and 1,600. In total, there are about 16,000 hospital beds in Alabama. Most of those are already at use today, and a growing outbreak of coronavirus will undoubtedly put a strain on Alabama’s hospital system.
Just how bad that strain will get is not yet known. Experts have said that more than 50 percent of the population could become infected with COVID-19—some have placed that number higher at 70 percent. Research out of China indicates that about 15 percent of people who are infected require hospitalization and about five percent require intensive care. Alabama has a population of 4.8 million. So at some point, 120,000 could require intensive care in the state and 360,000 could require hospitalization.
Of course, all of those cases won’t happen at once, but the number illustrates the importance of reducing the rate at which cases multiply across the state.
Harris, during the press conference on Monday, said there is no reason to be worried yet.
“Do we have enough beds and ventilators? Yes, we have been tracking the number of our bed capacity and our ventilators for about a week now using the Alabama Incident Management System,” Harris said. “At this time, we do not have any hospitals that are having issues with surge capacity that we’re aware of. And we track that daily. So we don’t think that’s an issue at the moment. Clearly, that’s always a concern when you’re dealing with a respiratory illness like this, and so we’ll continue to monitor that.”
This story will be updated.
Transcript of the Q&A
Q: This is Chip Brownlee with the Alabama Political Reporter. Dr. Marrazzo, I was wondering if you were—how you feel about the way that the state has handled this so far. And also, what’s your read on the preparedness level in terms of ventilators? I know you just talked about that. But do have any concerns, for Alabama in particular, that we’ll have enough ICU beds and ventilators to handle the cases?
Marrazzo: Sure. Great, great questions. I think that the governor has taken it very seriously. She’s convened a task force of which I’m a member and Dr. Harris is the leader. We’ve met several times in the last several days and I have a call actually, at one o’clock today. They have been—the leadership has been incredibly receptive to our suggestions and our feedback. So I think based on the state of emergency that was declared last Friday, the administration has been very responsive. I do think that as you’ll hear more emphasis particularly, particularly from local health departments like Jefferson County, on some of the more aggressive social-distancing measures, that the state government is going to need to amplify those messages.
You know, you saw all the pictures of people partying this weekend for St. Patrick’s Day, all the invulnerable people out there at the bars. I’m happy for them. But I’m very worried for us. I really don’t think people should be out doing that right now. And we all have to give a little bit to protect our community. So that’s a really important message. And I think the governor will be very on board with that, given the data.
Your second question about ventilators is a great one. We have, for example, at UAB hospital, I think it’s about 300 ventilators. So we have a lot. Is that going to be enough? In Italy, they don’t have enough. They are actually having to make decisions about taking people they believe are not going to survive off ventilators to reassign them to people. We do not want to be placed in that excruciating situation. It’s about the worst possible thing I can imagine as a physician talking to a family about that or dealing with that. I don’t believe there’s any indication we’re going to get there.
But again, my assurance is all based on my belief that we can deflect this curve and not be where Italy is right now. There are I like your question about the rest of the state though because we well know that many rural hospitals have been closing, right. We’ve been losing a lot of our smaller hospitals, even those that have remained open, may not have a deep staff to take care of critically ill patients. That’s when things do get frightening, and you do need to think about expanding your capacity at a place like UAB or a central place. We have contingency plans that we have been discussing. So this is basic disaster preparedness that people are actively pursuing. But I want to reassure people, we’re definitely not there. And we will be keeping very close, close track of this and updating you all as it comes on.
Q: This is Chip again, I’m wondering what you think about—some people have suggested that some of the hospitals across the state that have closed might need to be reopened. I’m wondering, given your experience, how likely you think that would be to happen, like, what would, what would those places have to do to reopen to deal with this?
Marrazzo: Yeah, I mean, it’s a great question and I think anything’s on the table right now. If we come to that point, and again, we should have much more data in hand over the next week, I would say. If we come to that point, you know, what that means is we’re looking at capacity beyond our immediate medical systems. That means either repurposing existing facilities or creating temporary new facilities, which is also a pretty heavy lift. What would have to happen is you’d have to obviously make sure the infrastructures were capable. And you’d have to more importantly, almost staff them up with people who are capable and willing to do that. So that’s a pretty big step people are, I know, in active discussions about that contingency planning as part of the disaster preparedness response. It’s really no different than thinking about a mass casualty like you might have with a hurricane or an earthquake or something like that. Unfortunately, you have an infectious disease, so it’s a little bit more dynamic and ongoing than either of those things. But I do know that people are talking about it and we will be updating you all as those discussions proceed and if they do proceed to anything more concrete.