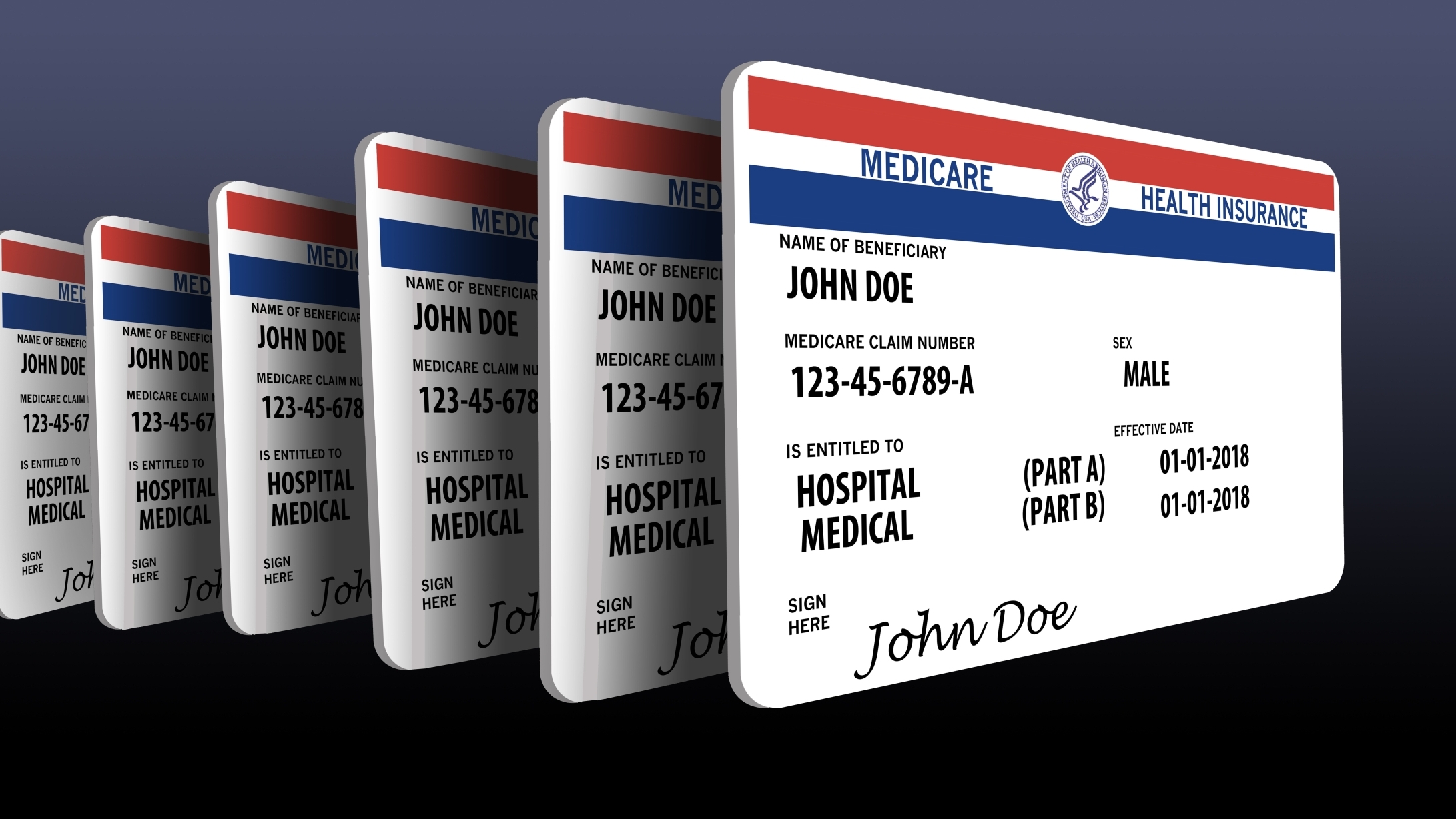
A report released by the Commonwealth Fund on Thursday placed Alabama’s Medicare performance among the ten worst states nationwide.
The healthcare research nonprofit’s State Scorecard on Medicare Performance ranks the quality and availability of Medicare care across states and D.C. based on 31 health system performance indicators, constructed from data gathered from 2023 to 2025 by public agencies, such as the Centers for Medicare and Medicaid Services.
States’ performance indicators for the federally administered program were organized into four performance domains: access to care, quality of care, affordability and population health.
Vermont, Utah and Minnesota topped the organization’s ranking for strongest Medicare performance across the four categories.
Meanwhile, Alabama ranked 44th in terms of combined performance domain rankings.
Alabama also came in as the state with the highest rate of 2023 Medicare beneficiaries with three or more chronic conditions, with 72 percent of enrollees having experienced three or more chronic conditions, such as diabetes or high blood pressure.
“Each state’s health care infrastructure is unique, making access to doctors and hospitals easier in some places than others,” the report reads. “Practice norms of local health systems and providers differ as well, meaning there is variation in which tests or treatments are commonly provided for a given condition.”
The Commonwealth Fund cited that one in five Americans is enrolled in Medicare.
Alabama ranked as the state with the 18th highest rate of overall Medicare enrollment, with 21.8 percent of Alabamians enrolled in the program in March 2025. Alabama also had the 4th highest rate of enrollment in Medicare Advantage, a type of Medicare plan offered by private companies with government authorization.
The study emphasized that although Medicare Advantage plans often cover some transportation to medical appointments, unlike traditional Medicare, the plans generally offer more restrictive access to provider networks, and most Advantage plans require prior authorization from insurers for certain services and medications.
“While prior authorization requirements may help to reduce inappropriate care or low-value services, they can also erect barriers to care for Medicare beneficiaries by delaying care, causing care disruptions, or denying medically necessary services,” the report stated.
In Alabama, prior authorization is required for certain services and prescription drugs by private insurers that offer Medicare Advantage coverage, although specific requirements vary from insurer to insurer.
The Commonwealth Fund reported that Alabama had a below average rate of prior authorization requirements for Advantage plans in February 2025. Compared to the national average of 48 percent, in Alabama, 42.4 percent of Advantage plans require prior authorization for specialist doctor visits or preventative care services.
Alabama ranked above the national average of Medicare beneficiaries enrolled in the Part D Low-Income Subsidy program, which helps low-income individuals pay prescription drug premiums and cost-sharing expenses.
In the state, 23.2 percent of beneficiaries were enrolled in the Part D program in February 2025, compared to a national average of 20 percent, or one in five Medicare enrollees.
Although Alabama received above average scores for several access to care indicators, such as the rate of patients who have a usual care provider, and the percentage of patients 65 years old or older who reported having a routine check-up in 2024, the state scored below average on all but one of the report’s quality of care indicators.
For instance, Alabama ranked as the state with the 3rd highest rate of Medicare beneficiaries 65 years old or older who received at least one drug that should be avoided by elderly patients, with 28.8 percent of such patients receiving high-risk medications in 2023.
The use of high-risk drugs by patients over 65 was found to be most prevalent in southeastern states, with Louisiana, Florida, Arkansas, West Virginia, Mississippi, Kentucky, Georgia and Tennessee also ranking in the top ten.
The study also found that potentially preventable hospital admissions occurred twice as often in 2023 among states with low performing Medicare programs, when compared to the best performing states.
Alabama had the 3rd highest rate of preventable hospital admissions, with roughly 32 out of 1,000 Medicare beneficiaries being admitted to a hospital for ambulatory care-sensitive conditions, or conditions that could have instead been managed by a doctor’s office or clinic visit.
The report found that states with the lowest life expectancy averages for 65-year-olds were among those that spent the most per traditional Medicare beneficiary.
The Commonwealth Fund cited that, in 2023, Alabama tied with Kentucky and Oklahoma for an average life expectancy of 16.4 years for 65-year-olds. Only West Virginia and Mississippi reported lower life expectancy averages of 16.1 years.
Alabama had the overall 6th highest spending per traditional Medicare beneficiary with $13,002 per enrollee in 2023.
“As a nation, the U.S. consistently spends more on health care than its peers around the world yet has lower life expectancy at birth,” the report reads. “Why is a question that has long vexed policymakers. We do know that life expectancy at age 65 is a product of many factors, including the medical care and nonmedical services people get both before and after Medicare enrollment.”
Alabama scored poorly in overall medical care affordability for both Medicare eligible and non-eligible patients; however, the state’s Part D program paid higher than average percentages of prescription drug costs for patients in 2025.
The state had the 11th highest rate of Medicare-eligible adults 65 years old or older who went without medical care in 2024 due to the cost, with 4.3 percent. Meanwhile, Alabama reported the 7th highest rate of individuals aged 18 to 64 who opted to go without care due to financial reasons, at 17.3 percent.
D.C. featured the lowest average rate of Part D beneficiary drug payments at 3 percent, while Alabama had the 11th lowest prescription drug expense rate for Part D recipients, with an average of 6.3 percent, compared to the national average of 7 percent.
“This scorecard highlights both Medicare’s remarkable impact and the urgent need to ensure it delivers care equally and effectively for people in every state,” Commonwealth Fund President Dr. Joseph R. Betancourt wrote of the report.
“The quality of care received by Medicare recipients is very dependent on the ability to access care in Alabama. Our health care infrastructure has been in a financial crisis for years, with providers leaving rural areas,” AARP Alabama Associate State Director of Communications Jamie Harding told APR in response to the study.
“This means fewer options for many Alabamians, who then have to travel longer distances to find care,” Harding added. “And then transportation can become an issue as well. Solving the challenges in accessing care requires a comprehensive strategy from Alabama’s leaders.”
In their overview of variations in statewide health outcomes for Medicare recipients, the Commonwealth Fund called for federal policymakers to ensure “clear Medicare coverage rules” and “appropriate payments to providers.”
The organization also called for policymakers to “incentivize providers to apply best practices and reduce wasteful care” and to enhance Medicare programs for low-income Americans, such as Part D and the Medicare Savings Programs.
“It’s noteworthy that Medicare performs better in states where the health care system also performs better for other populations,” the Commonwealth Fund wrote. “In fact, the top performers in this report overlap with many of the highest-ranking states in other assessments of health care system quality and performance.”
“Clearly, a state’s health care infrastructure, its clinical practice norms, and its policies affect all state residents, including Medicare beneficiaries, and investments in the health care system benefit everyone,” the report continued. “This confluence of state and federal health policy is what enables beneficiaries to get the health care they need and ultimately affects their health outcomes and experiences with health care.”