In rural Alabama, proximity shapes everything. Hospital leaders, plant managers, clinicians and county officials see each other regularly. A problem noticed on Monday might be discussed by Friday. That closeness does not solve all challenges, but it helps communities learn and adjust faster when people pay attention.
This sense of connection is part of what keeps rural Alabama going. Communities endure by adapting, even when resources are stretched and pressures mount. But grit alone is not enough. Endurance works best with clear sight, when leaders can spot strain early and notice what is quietly slipping away.
Take a rural hospital administrator who keeps a small notebook on her desk. Each month, she records the same things: how long patients wait, how many emergency transfers might have been avoided, how many nurses leave for better pay elsewhere.
What began as preparation for board meetings became something more. A record of what her community was slowly losing.
Those notes tell stories good intentions cannot. They reveal whether reforms are helping people or just moving money. Patterns surface early, before they harden into crises. When shared across clinics, hospitals, employers, and insurers, these insights create a common language for solving problems that too often remain isolated.
The Alabama Rural Health Transformation Program is moving from approval into action. Some partnerships will thrive; others may strain. Success will not come from vision statements or press releases. It depends on whether leaders see what is happening soon enough to learn and adjust.
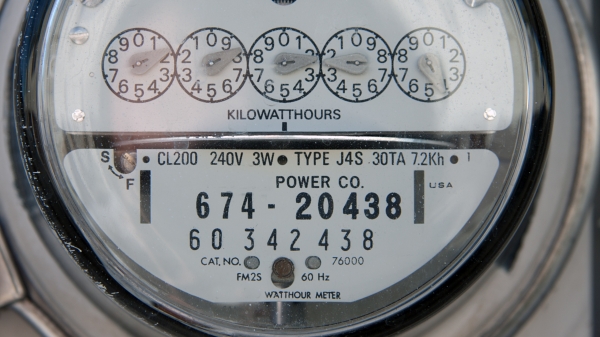
Rural health systems live close to the edge. A delayed insurance payment can affect payroll in weeks. A nurse leaving shows up almost immediately as longer wait times. Yet many decisions rely on partial or outdated information. Patient counts that miss timing. Claims data arriving too late to guide the next season. Reports that document activity but do not show if care improved.
The answer is not more paperwork. It is smarter feedback.
Alabama needs two kinds of attention. Some efforts require a clear look back to judge if they worked. Others need steady, built-in ways to learn and adjust day to day. One helps leaders decide what to keep or change. The other helps frontline teams improve without waiting for a final verdict. Both matter. Confusing them weakens each.
When hospitals, clinics, employers and insurers track a small set of shared signals, real-time improvement becomes possible. Real experiences show how this works. A plant manager notices fewer missed shifts tied to unmanaged chronic illness and asks what changed. For rural employers, even a few absences can disrupt a production line, strain workers and threaten tight margins. A clinic sees faster recovery after tightening care coordination and shares what worked. An insurer spots steadier claims and fewer costly interventions. Learning spreads because everyone sees the same picture.
For leaders sorting through all this, questions like these matter more than any dashboard:
- Are we tracking what helps people make better decisions, or just what is easiest to count? Measures should clarify trade-offs, not just record activity.
- Do these signals reflect what patients, staff, and employers experience? Indicators matter most when people on the ground recognize them as real.
- Are we paying attention both to results and whether changes are used? When outcomes disappoint, the problem often lies in fit or follow-through, not the idea.
- Is the effort to collect information worth the insight it gives locally? Measures that drain time without improving care erode trust fast.
- Are we looking often enough to learn before problems get worse? Timely feedback supports improvement. Delayed data turns evaluation into history.
- Do these measures encourage better care, or might they quietly distort behavior? Balanced signals help avoid trading speed for quality or volume for value.
Learning spreads because everyone sees the same picture. But getting there means tackling the toughest challenge: building trust in measurement.
Trust is harder to earn than any dashboard. Health care workers already feel buried in paperwork that often seems far from patients. Adding measures that offer no local value invites pushback. Rural providers know their patients are older, sicker and harder to serve. Measurement that ignores that feels punitive, even if it is not meant to be.
Good measurement begins with respect for local realities. Rural systems begin from different places. Some have steady staffing; others do not. Some have broadband and specialists nearby; others rely on long drives and small teams. Measures that ignore those differences do not improve care. They weaken confidence.
Technical barriers remain. Rural providers use different record systems. Claims and clinical data rarely align neatly. Employers cannot access personal health information. State systems were not built to connect easily, though Alabama’s One Health Record initiative aims to address this over time. Meanwhile, progress will be slow. Simple tools, regular talks and shared spreadsheets can support learning while bigger systems improve.
Here again, proximity helps. In rural Alabama, a county health leader can call a plant manager and compare notes within days. Small adjustments happen faster. When progress is visible, confidence grows.
That visibility matters politically. It shows public dollars working without noise or blame. It gives legislators, agency leaders and local boards steady proof when questions come.
Principles only become real when people can see them at work. Transparency depends on information people trust. Accountability depends on results that are visible. Sustainability depends on showing value over time. Trust grows when learning replaces blame. Predictability comes from steady signals, not surprises.
Rural Alabama has always known how to make do with less. That spirit can guide measurement that is lean, practical, and focused on what matters. The administrator with the notebook already understands this. The challenge now is turning individual discipline into shared strength.
When communities clearly see their own progress, reform stops being abstract policy. It becomes something people believe in because they can point to it. That belief, grounded in facts, not hope, is what sustains reform when the initial excitement fades and the hard work of execution begins.
David L. Albright, PhD, is a University Distinguished Professor at The University of Alabama, a board member of the DCH Healthcare Authority, and immediate past president of the Alabama Rural Health Association. The views expressed are his own and do not necessarily reflect those of his institution or affiliated organizations.