The Senate Healthcare Standing Committee considered a bill that would require Alabama hospital emergency rooms to be staffed by a physician at all times and drew strong support from emergency medicine doctors and sharp concern from some lawmakers.
SB80, sponsored by Sen. Larry Stutts, R-Tuscumbia, would mandate that a licensed physician be physically present and primarily responsible for patient care in hospital emergency departments. The legislation, Stutts said, reflects what most Alabamians already expect when they seek emergency medical care.
“This bill simply is only two pages long and just requires that hospital emergency rooms are staffed by a physician. I think that is the expectation of the general public. When you go to an emergency room, you expect to have somebody there qualified to take care of you,” said Stutts.
Stutts, a physician himself, pushed back against arguments from the hospital industry that the requirement would be too costly.
Drawing on his own experience working in rural emergency rooms, Stutts described situations where immediate physician care made the difference between life and death.
“I can tell you that there were several times during those moonlighting experiences that had somebody not been there, qualified to take care of the patient, that rolled in the door, there would not have been a good outcome,” said Stutts.
Emergency physicians testified in support of the bill, arguing that physician-led care is essential in unpredictable, high-risk emergencies, particularly in rural hospitals where specialty backup is often unavailable.
Dr. Sean Vanlandingham, an emergency physician and president of the Alabama Chapter of the American College of Emergency Physicians, explained that the bill is not an indictment of nurse practitioners or physician assistants, but rather a recognition of differences in training.
“Physicians complete four years of medical school, three years or more of residency, and accumulate 12,000 hours or more of supervised patient care,” said Vanlandingham. “By comparison, nurse practitioners typically complete about 500 clinical hours. That difference matters most when patients are critically ill.”
Vanlandingham warned that allowing emergency departments to operate without physicians creates unequal standards of care based solely on geography.
“When emergency departments operate without a physician present, patient outcomes suffer, and disparities increase. This is especially true in rural hospitals, where there are no surgeons, no OB-GYNs, no other specialists to provide backup,” said Vanlandingham.
Dr. Jared Raper, president-elect of the Alabama Chapter of the American College of Emergency Physicians, addressed concerns that the bill could force rural hospitals to close, pointing to other states that have adopted similar requirements.
“South Carolina, Indiana, and Virginia have all passed physician presence requirements beginning in 2023,” said Raper. “To date, none of those hospitals have had to close as a result of this legislation.”
Raper also argued that physician absence can actually increase costs by driving unnecessary testing and transfers.
“In complex, high-acuity cases, uncertainty often leads to more labs, more CT scans, more transfers, and ultimately, more downstream costs. Those costs are real, and they’re gonna be borne by the patients as well as the hospitals that care for them,” said Raper.
Despite the medical community’s support, some lawmakers raised concerns about the bill’s potential impact on rural and critical access hospitals already struggling to remain open.
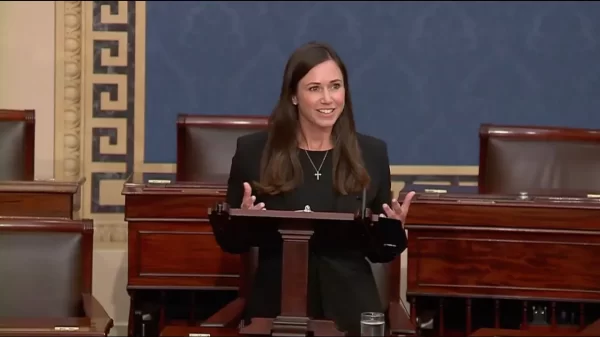
Senator April Weaver, R-Brierfield, said she could not support SB80, citing her work on the Alabama Rural Roadmap initiative and concerns about imposing stricter requirements than those set by the federal government.
“We are making them have a regulation that the federal government does not make them have,” said Weaver. “Why would we have stricter regulations than what’s coming down from the federal government?”
Weaver warned that the bill could unintentionally penalize rural facilities where a single physician may be responsible for multiple duties.
“There was a situation where the ER doctor may have to go to the nursing home to pronounce someone dead, or he may have to run across the street real quick to the specialty clinic for something. And this on-site here, I mean, it would be against the law in a situation like this, when there’s that one provider there that’s doing multiple jobs,” said Weaver.
Committee members ultimately did not vote on the legislation. The bill would be held over for further consideration.