UPDATE: The owner of the largest bar in Auburn has said they will not reopen this week, according to The Auburn Plainsman.
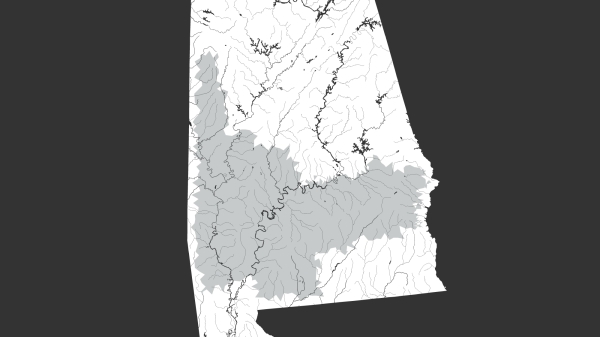
Lee County, Alabama—the home of Auburn University, where officials have been having trouble discouraging young people from visiting bars—now has the second-highest number of COVID-19 cases in Alabama.
The Alabama Department of Public Health reported four new cases in Lee County Wednesday, bringing the county’s total up to seven. While it’s unclear where the cases were reported within the county, Auburn is the largest city.
The city is also home to a growing retirement community and thousands of college students who, according to data from outbreaks around the globe, are more likely asymptomatic carriers of the virus. Young people tend to survive the infection, but can spread it more easily.
[visual-link-preview encoded=”eyJ0eXBlIjoiaW50ZXJuYWwiLCJwb3N0Ijo4MzEwOSwicG9zdF9sYWJlbCI6IlBhZ2UgODMxMDkgLSBNYXBwaW5nIENPVklELTE5IGluIEFsYWJhbWEiLCJ1cmwiOiIiLCJpbWFnZV9pZCI6ODMwNzYsImltYWdlX3VybCI6Imh0dHBzOi8vd3d3LmFscmVwb3J0ZXIuY29tL3dwLWNvbnRlbnQvdXBsb2Fkcy8yMDIwLzAzL0Fkb2JlU3RvY2tfMzE4OTg5NTYyLXNjYWxlZC1lMTU4NDEzNzY2MzIwMi0xMDAweDYwMC5qcGVnIiwidGl0bGUiOiJNYXBwaW5nIENPVklELTE5IGluIEFsYWJhbWEiLCJzdW1tYXJ5IjoiV2UncmUgbWFwcGluZyB0aGUgb3V0YnJlYWsgaW4gQWxhYmFtYS4iLCJ0ZW1wbGF0ZSI6InVzZV9kZWZhdWx0X2Zyb21fc2V0dGluZ3MifQ==”]
One new case was reported in Calhoun County. Two new confirmed cases are in Jefferson County, which has a total of 23 confirmed cases and the state’s largest number. But these numbers have a lag time. It’s taking at least 24 hours and sometimes several days to get results from the time when people are tested.
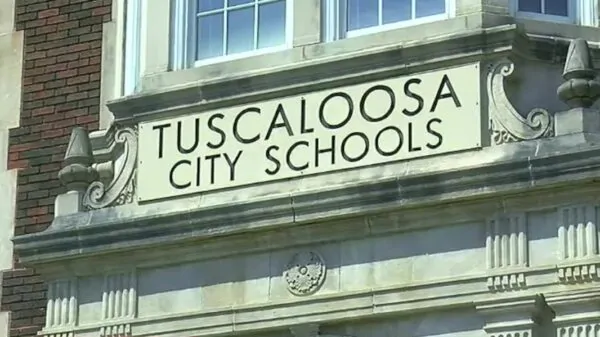
A lot of people have been having trouble getting access to tests. The testing centers in Birmingham are so swamped that they’ve closed just a few hours after they opened. A testing site in Tuscaloosa at DCH Regional Medical Center has been having better luck.
EAMC, the hospital nearest Auburn, has been getting hundreds of calls a day but, by Tuesday night, had only been able to test 100 people because of limited supplies and high demand.
[visual-link-preview encoded=”eyJ0eXBlIjoiaW50ZXJuYWwiLCJwb3N0Ijo4MzY4MywicG9zdF9sYWJlbCI6IlBhZ2UgODM2ODMgLSBUaGVzZSBjaGFydHMgc2hvdyBob3cgQWxhYmFtYSdzIGhvc3BpdGFscyBjb3VsZCBiZSBvdmVyd2hlbG1lZCIsInVybCI6IiIsImltYWdlX2lkIjo4MzIwMCwiaW1hZ2VfdXJsIjoiaHR0cHM6Ly93d3cuYWxyZXBvcnRlci5jb20vd3AtY29udGVudC91cGxvYWRzLzIwMjAvMDMvQWRvYmVTdG9ja18xODk2ODExNzEtc2NhbGVkLWUxNTg0MjM4NzQ5MzUwLTEwMDB4NjAwLmpwZWciLCJ0aXRsZSI6IlRoZXNlIGNoYXJ0cyBzaG93IGhvdyBBbGFiYW1hJ3MgaG9zcGl0YWxzIGNvdWxkIGJlIG92ZXJ3aGVsbWVkIiwic3VtbWFyeSI6IkNhbiB0aGV5IGhhbmRsZSB0aGUgc3RyYWluPyIsInRlbXBsYXRlIjoidXNlX2RlZmF1bHRfZnJvbV9zZXR0aW5ncyJ9″]
Gov. Kay Ivey and the Department of Public Health announced Tuesday that six Central Alabama would face more restrictions. Bars and restaurants are now limited to take-out service and all private schools and daycares have been closed. So far, these restrictions have not been extended to Lee County, but officials are likely to re-evaluate and expand them across the state if spread continues.
Videos have been posted of some of the largest bars in Auburn measuring temperatures using an infrared thermometer as young people enter the bar.
https://twitter.com/PabloEscobarner/status/1240302715370196992
But officials have warned that those who are infected can be contagious for more than a week before they begin to show symptoms, which include a fever. The average incubation time between infection and the emergence of symptoms is five days, according to the World Health Organization.
Dr. Deborah Birx, the White House’s coronavirus response coordinator, said Tuesday that young people are getting sick and disproportionately infected in Europe. Many are being hospitalized. Birx said it appears to be because young people heard that the elderly are more vulnerable—a data point based on data out of China—and they are ignoring public health guidance.
“We are aware that there are several businesses in Auburn that are promoting St. Patrick’s Day celebrations,” City Manager James Buston told WSFA. But “the city council of the City of Auburn does not have the authority to force them to close.”
https://www.facebook.com/CityofAuburnAL/videos/252155275795065/