Alabama State Health Officer Dr. Scott Harris said Thursday that the spike in new COVID-19 cases over the last two weeks is not totally attributable to increased testing and that the Alabama Department of Public Health believes there is ongoing, widespread community transmission of the virus.
“We’re extraordinarily concerned about the numbers that we have been seeing,” Harris said. “We know that ADPH and partners we work with have managed to increase the number of tests we’re doing throughout the state, but that doesn’t account for the case numbers that we’re seeing, or certainly doesn’t completely account for it.”
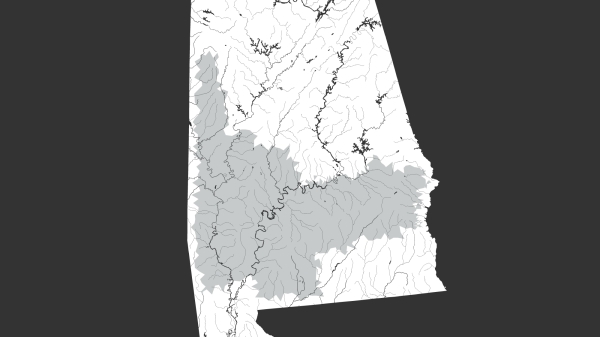
Harris said the state has identified a number of growing hotspots, including in Montgomery County, Tuscaloosa County and Walker County, where spikes in cases are not attributable to increased testing but rather outbreaks connected to businesses, nursing homes and widespread community transmission.
“We know that we continue to have community transmission going on in many parts of the state,” Harris said on a Facebook town hall with U.S. Rep. Terri Sewell. “We certainly identified many hotspots. …Sometimes we understand the reasons. Sometimes we do not. But clearly there’s a lot of disease transmission still going on.”
Harris said the increased daily case counts — which are increasing faster than 46 other states — should serve as a reminder that social-distancing recommendations must be followed, people must wear masks when out in public and people should avoid large crowds, even if those actions are not mandated by the government.
“Now more than ever, now that people are out in public, this is the time when they really need to follow those rules, those guidelines,” Harris said. “We need people to stay six feet apart, or more, from folks who aren’t in their own household. When people are going out into public, and particularly in indoors, perhaps into businesses or in other places, where they’re mixing with other people, face coverings, mask of some kind, are imperative and absolutely everyone needs to do that.”
The state health officer, who leads Alabama’s Department of Public Health, said the state was very concerned by photos and videos of massive crowds not wearing masks on Alabama’s beaches and Gulf restaurants over Memorial Day weekend.
“We did not like that at all,” Harris said. “I had conversations with local officials there about them and they certainly recognize and understand the dangers of that as well. They have done their best to use law enforcement to try to enforce that to the extent they can. But ultimately, we need the public to accept this. And to do this, we need the public to buy in and understand.”
Over the past two weeks, Alabama has confirmed an additional 5,080 cases, bringing the total number of confirmed cases up to 16,181. About a third of the state’s cases have been confirmed in the two weeks since the state relaxed restrictions on bars and restaurants on May 11.
{{CODE1}}
Seven- and 14-day rolling averages, used to smooth out daily variability in reporting, are higher than during any point in the outbreak, meaning more new cases per day are being confirmed than ever before.
{{CODE2}}
There has been no comparable increase in testing. Alabama broke 200,000 total tests performed on Thursday. But over the past 14 days, about 4,004 tests per day have been performed, on average. Over the previous 14-day period, ending May 14, the average number of tests per day was roughly the same at 4,032.
{{CODE3}}
Meanwhile, the percent of tests that are positive has been rising after dropping to as low as 3 percent on May 1, based on 7-day averages of increases in tests and cases. The same metric rose to 10 percent by Wednesday.
{{CODE4}}
Over the last 14 days, at least 117 people have died from COVID-19. On Thursday, the number of deaths attributable to the virus rose to 590.
{{CODE5}}
“Those numbers do sound like numbers, they’re statistics,” Harris said on another Facebook town hall with Sen. Doug Jones. “But it’s really important to remember that every one of those numbers is a person. They’re someone’s parent or child or brother or sister. And so we never want to lose sight of the fact that we are having Alabamians who are dying from COVID-19 disease.”
Harris said the rise in cases is worrisome, and the state expected some rise after lifting the state’s stay-at-home order and loosening restrictions on businesses and gatherings.
“We’re going to need people to be more careful than ever,” Harris said.
Harris repeatedly emphasized the importance of wearing masks when out in public and said maybe public health officials need to do more to emphasize the importance of masks.
“People feel like a mask just protects me, and if I’m not worried about getting sick, then why should I wear a mask?” Harris said. “But a mask is how you protect other people.”
A mask controls your own coughing or sneezing or other symptoms — or just transmitting it because you’re talking or yelling or spitting. Such precautions are important because at least a quarter of people and maybe as many as a third of people who are infected and can infect others won’t have any symptoms at all.
“So, it’s certainly possible that you can be infectious to other people and not even know it,” Harris said. “So that’s what a mask is for. A mask, in my mind, is good manners. A mask is how you show that you care about people in your family or in your community, particularly those people who are very vulnerable, or seniors or people with chronic health problems.”
Masks are also important even when not around vulnerable people because you could spread the virus to someone else, who then unwittingly could spread it to a nursing home or extended care facility.
In Tuscaloosa County, DCH Health System has seen the number of hospitalizations from COVID-19 more than double over the course of a week, in part because of an outbreak at a long-term care facility in the county and in part because of community spread, Harris said.
Similar outbreaks at long-term care facilities in Elmore County, Butler County and a workplace in Walker County and Franklin County have contributed to rising numbers, Harris said.
[visual-link-preview encoded=”eyJ0eXBlIjoiaW50ZXJuYWwiLCJwb3N0Ijo4MzEwOSwicG9zdF9sYWJlbCI6IlBhZ2UgODMxMDkgLSBNYXBwaW5nIENPVklELTE5IGluIEFsYWJhbWEiLCJ1cmwiOiIiLCJpbWFnZV9pZCI6ODczMTEsImltYWdlX3VybCI6Imh0dHBzOi8vd3d3LmFscmVwb3J0ZXIuY29tL3dwLWNvbnRlbnQvdXBsb2Fkcy8yMDIwLzA0L0Fkb2JlU3RvY2tfMzM0NDI3OTI4LTEwMDB4NjAwLmpwZWciLCJ0aXRsZSI6Ik1hcHBpbmcgQ09WSUQtMTkgaW4gQWxhYmFtYSIsInN1bW1hcnkiOiJZb3UgY2FuIHNlZSBjb3VudHktYnktY291bnR5IGRhdGEgb24gb3VyIGRhdGEgYW5kIG1hcHBpbmcgZGFzaGJvYXJkLiIsInRlbXBsYXRlIjoidXNlX2RlZmF1bHRfZnJvbV9zZXR0aW5ncyJ9″]
“Some of those are outbreaks,” Harris said, “and yet again, those are still attributable to community spread. The people in the nursing home didn’t go out into the community and catch it. Someone brought it into them. There has to be transmission going on in the community for that to happen. We need to find a way to get people to take this seriously.”
Harris said the Department of Public Health is not aware of any particular origin for the rising cases in Montgomery County, however, and that officials believe the rise is largely due to widespread community transmission and in part due to increased testing.
But the increase in cases also accompanies a rise in the percent of tests that are positive in Montgomery County, despite increased testing there. There has been some controversy about Montgomery Mayor Steven Reed saying no ICU beds were available in the city, but Harris said he was “absolutely correct.”
“There were no ICU beds available,” Harris said. “We talked to the hospitals immediately upon learning about that. I think their response was that that’s correct. However, they do have some internal capacity, when they need to do it, to expand the space that they have available and take care of critically ill patients.”
In Montgomery, that has involved treating critically ill patients in emergency rooms and retrofitted ICU units, a Montgomery area doctor told APR earlier this week. But there remains a shortage of ICU beds.
“I think that the message that we want to be careful about putting out there is: clearly those hospitals have higher numbers, they have you know their normal beds filled, and yet the public sometimes hears that and thinks well if I have a heart attack, I don’t have a place to go or they’re going to turn me away if I show up because the hospital’s full, and that’s not the case,” Harris said. “And so we want people to understand they certainly still can continue to seek care, just as they always would for any kind of a problem. They should do that. They certainly shouldn’t try to sit at home if they’re concerned about a certain thing.”
But if numbers continue to rise, the situation could become a dire problem.
“If numbers go up, they can’t do that forever, and then we’ll have to have to make other arrangements,” Harris said.