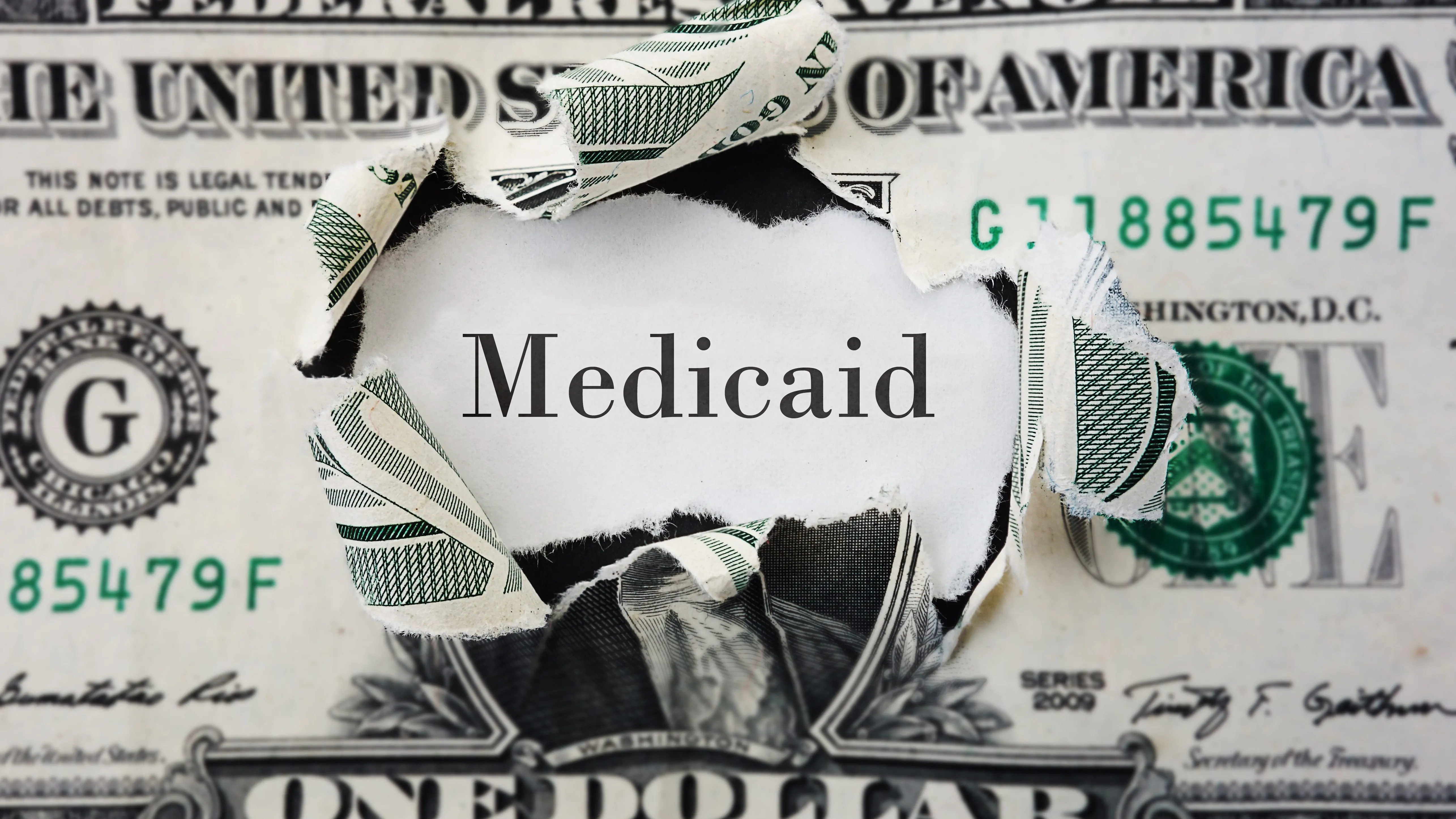
Last week, President Donald Trump signed into law the “One Big Beautiful Bill Act,” a massive piece of legislation which, among other things, levies severe cuts to federal spending on Medicaid, increases eligibility requirements for Medicaid coverage, and shifts costs of funding and administering Medicaid from the federal government to the states.
On Wednesday, APR spoke with Louise Norris, the lead writer for healthinsurance.org—an independent source on the Affordable Care Act and Medicaid policy—to better understand the incoming effects of the OBBBA on Medicaid in Alabama and across the country.
Norris began our conversation by dispelling some of the misinformation used by Republican lawmakers to justify their cuts to Medicaid and the expansion of work requirements for individuals living in Medicaid expansion states.
“The biggest Medicaid cut is going to be the work requirements that kick in in 2027… The people writing this bill were framing it as if there are millions of people who are on Medicaid just sitting around playing video games not working and that somehow this bill will get them working and fill in empty jobs… In reality, most people on Medicaid, most adults on Medicaid, who are not elderly, are already working or they have barriers to work, such as they are a caregiver for a small child or for an elderly parent, or they are chronically ill,” Norris said.
“It’s a very small percentage of adults on Medicaid who could be working but aren’t, and some of those are people who are, maybe they’re 63 years old and they’ve retired, but they’re not eligible for Medicare yet,” she added. “Theoretically, those are people that this work requirement [would target]—I mean it will target them—but it’s not really all that practical to say, ‘okay, a 63-year-old who’s retired now needs to go back to work until they qualify for Medicare,’ because oftentimes those folks have retired because of chronic health conditions that are keeping them out of the workforce. So that is a big misconception.”
Norris also clarified that these additional work requirements will impact more than just able-bodied adults on Medicaid, as states are forced to find areas to cut Medicaid spending due to decreased federal dollars.
“I think another misconception is this idea that it will only target able-bodied adults when in reality when you’re taking a trillion dollars out of the Medicaid system over a decade, that’s going to have ripple effects to everyone on Medicaid, just in terms of states having to figure out how to balance their Medicaid budgets and making cuts either to eligibility or to benefits,” she said. “Optional benefits like home- and community-based services that provide in-home care for people who are chronically ill or disabled or elderly, there could certainly be cuts to programs like that as states work to offset the budgetary impacts.”
It is important to note that these additional work requirements will not affect the 10 states, including Alabama, that have yet to expand Medicaid through the Affordable Care Act, because they were already missing out on the federal dollars offered through Medicaid expansion.
“In a state like Alabama where they haven’t expanded Medicaid, there won’t be a new work requirement because Medicaid isn’t expanded. So, the budgetary impact of the work requirement won’t apply in states like Alabama, which means their overall budget cuts to Medicaid will be lower… but that’s because Alabama has already been missing out on all this federal funding. All the states that expanded Medicaid back in 2014, or at any point since then, have been getting a whole lot of extra federal funding for their Medicaid programs,” Norris explained.
However, Norris told APR that where Alabamians won’t be hurt by the new Medicaid work requirements, they will be hurt by the OBBBA’s failure to extend the ACA premium tax credit, which will result in less affordable marketplace coverage.
“Where there will be a bigger impact, a disproportionate impact, will be the ending of the enhanced premium subsidies in the marketplace at the end of this year, assuming Congress doesn’t take action to address that,” she continued. “In states that expanded Medicaid, people up to 138 percent of the poverty level qualify for Medicaid, whereas in a state like Alabama, if you are below 100 percent of the poverty level and you’re an adult, you just don’t qualify for anything, but if you’re above 100 percent of the poverty level, you qualify for very significant subsidies in the marketplace. There’s an overlap there—the people between 100 and 138 percent of the poverty level—so it’s a pretty low-income population. In most states, those folks are on Medicaid and are going to be subject to new work requirements, whereas in a state like Alabama, those folks are in the marketplace with basically what amounts to full subsidies at this point, they don’t have to pay anything for their coverage.”
“They can choose to upgrade to a higher level of coverage where they have premiums, but they currently qualify for quite a few zero-cost plans. That’s going to go away at the end of this year. And so, especially on that lower income end of the spectrum, we’ve seen huge gains in marketplace enrollment in states like Alabama that hadn’t expanded Medicaid and that’s expected to drop off next year,” Norris explained. “So the overall impact is going to be more people uninsured, it’s just [that] in Alabama, they’re going to go from having marketplace coverage to being uninsured, whereas in states that had expanded Medicaid, those lower income folks might go from having Medicaid to being uninsured.”
As for how the OBBB may impact Alabama’s ability to expand Medicaid in the future, Norris explained that added work requirements—which would incur increased administrative costs—and the elimination of Medicaid expansion incentives included in the 2021 American Rescue Plan Act could further disincentivize states like Alabama from expanding Medicaid.
“Back in 2021, the American Rescue Plan included a provision for states that still haven’t expanded Medicaid. If they did so after the American Rescue Plan was implemented, they got a two-year boost in their overall federal Medicaid funding,” Norris said. “The federal government [already] pays for 90 percent of the cost of covering [the expansion population], but what the American Rescue Plan did was boosted up the percentage of Medicaid costs that the federal government would pay for the rest of their Medicaid population. It’s only a two year thing, it’s not permanent, but it did help to just make it easier budgetarily for states.”
Although only three states—Missouri, North Carolina and Oklahoma—took advantage of the Medicaid expansion incentive in the American Rescue Plan, its elimination under the OBBB could still contribute to states like Alabama continuing to decline expansion as could the new federal work requirements.
“It obviously wasn’t serving as a huge incentive to get the holdout states to extend Medicaid, but if they were contemplating it, that’s no longer an option,” Norris said. “The other thing is that now, if [a state does] implement Medicaid expansion, it will have to be with a work requirement since these federal rules kick in in 2027. And, to be fair, in most of the 10 states that haven’t yet expanded Medicaid, work requirements have definitely been part of the discussion over the years when they’ve contemplated Medicaid expansion in the legislatures, it just hasn’t gone anywhere.”
Critics of the OBBB have also noted that its cuts to Medicaid could cause rural hospitals already operating on slim margins to shutter across the U.S. Just last week, a rural hospital in Southwest Nebraska announced that it would be shutting its doors, citing the anticipated federal budget cuts to Medicaid as one of the factors behind its closure.
Norris also highlighted the damage that the OBBB will deal to rural hospitals in Alabama and across the country, emphasizing that the closure of rural hospitals will have a negative ripple effect for providers and patients in urban areas as well.
“In areas where rural hospitals close, you still have that ripple effect out to all the other hospitals because the patients who were going to those hospitals that end up closing—or nursing home, or skilled nursing facility—the patients still need care, so obviously there’s an extra burden on those patients to get to the next closest facility. But then there’s extra strain on those facilities because they have to absorb additional patients,” Norris noted. “So it’s not just an issue of ‘are you in a community where facilities close or are you not?’ because of the ripple effect.”
Norris also stressed that hospitals taking on more uninsured patients due to loss of Medicaid coverage will end up shifting those increased costs to Americans covered by marketplace plans and private insurance in the form of higher premiums.
“The expectation is that—between this bill, the [2025 Marketplace Integrity and Affordability Final Rule] that was finalized last month, and then the fact that Congress hasn’t extended the marketplace subsidy enhancements—the overall expectation is 17,000,000 additional people becoming uninsured. And that impacts the whole health coverage system because that results in more uncompensated care in the hospitals,” Norris said. “They pass that cost on to commercially insured patients, so people with marketplace coverage, people with employer sponsored coverage, those premiums go up.”
“In the states where we’ve seen premiums for the individual market for next year, the proposed rates are [showing] more than 15 percent increases on average just to the base rates before any subsidies are applied. So that’s a pretty significant jump in premiums. So this does affect everyone, regardless of whether you’re on Medicaid or on a marketplace plan,” she added.
As for what Americans and Alabamians should do to prepare for these impacts, Norris stressed the importance of staying informed about changes to your healthcare plan, whether you are on Medicaid or not.
“I think the big takeaway here is really to pay attention to any communications you get from your health plan, from your state Medicaid agency, from the marketplace if you’re enrolled in a marketplace plan. Just pay close attention and understand that, going forward, some of these programs that you might have found it fairly easy to enroll in and keep your coverage in the past, there might be new administrative tasks you need to do to keep your coverage,” Norris stressed. “People just really need to be heads up about that.”