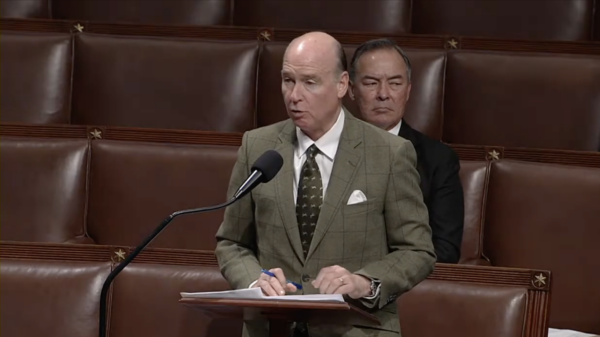
A U.S. Senate Committee on Veterans’ Affairs hearing convened in Alabama by U.S. Senator Tommy Tuberville, R-Alabama, on Friday examined emerging and alternative treatments for veterans’ mental health.
The hearing, which took place at American Village in Montevallo in a replica of the White House’s East Room, invited researchers and veteran advocates to explore the use of alternative therapies such as psychedelic drugs and hyperbaric oxygen in treating post-traumatic stress disorder and traumatic brain injuries among veterans.
“Unfortunately, what we are here to discuss is not new we lose an average of eighteen veterans a day to suicide,” Tuberville said. “And our veteran class is growing because of all these 20-year wars we’ve been fighting over the last few years.”
“We cannot sit back while those who put their lives on the line for our great nation suffer day in and day out; we have a lot of suffering,” the senator added.
Tuberville pointed to a bill he sponsored in March to expand access to hyperbaric oxygen therapy, known as HBOT, through the VA.
“I’m eager to hear how the VA is working to study and provide access for treatments outside of medication such as opioids, antidepressants and traditional psychotherapy,” the senator said in his opening remarks.
The forum opened with Tuberville hearing a statement from the U.S. Office of Mental Health’s Veterans Health Administration deputy director, Dr. Ilse Wiechers.
Wiechers announced that, as of July, the VA was conducting 12 clinical studies at nine VA research centers studying the merits of psilocybin, MDMA, DMT and LSD in the treatment of PTSD, major depressive disorder, generalized anxiety disorder and substance abuse disorders.
While Wiechers cited that VA had seen success in the use of psychedelics in PTSD and TBI treatment, the organization’s research did not indicate HBOT’s efficacy as a potential therapy.
“Although HBOT is recognized for conditions like decompression sickness and wound healing, the FDA has not authorized it for use with PTSD or TBI treatment,” she said. “VA and DOD clinical practice guidelines found insufficient evidence to recommend HBOT for PTSD and strongly recommend against its use for mild TBI.”
Wiechers was accompanied by the executive director of the Office of Research and Development’s Brain, Behavioral and Mental Health Portfolio, Dr. Miriam Smyth. The two researchers fielded questions from the senator regarding the VA’s clinical studies on psychedelics and HBOT for veterans.
Smyth explained to Tuberville that in order to conduct clinical research using controlled substances, which are federally illegal for individual possession, research institutions must receive FDA approval, a license from the DEA and complete inspections by institutional review boards.
When asked to describe misconceptions regarding psychedelic therapies, Wiechers told Tuberville that, unlike traditional take-home medications, VA clinical trials for therapies that include the use of psilocybin or ketamine occur at a VA clinic in a controlled environment regulated by medical professionals.
“These therapies remain investigational, and it is important to not self-medicate with psychedelics outside of a clinical research setting,” Wiechers said.
“It doesn’t work for everyone. It’s not a magic bullet, but the data looks good,” Wiechers said of psychedelic therapy for veterans suffering from PTSD or substance abuse disorders.
“For those whom it helps, it can help quite a bit,” the researcher added.
Tuberville pointed to his personal use of hyperbaric oxygen treatment, which he said he first learned of during his time as a football coach.
“We felt like it helped; it enhanced, cleared their mind to some point. I think my wife caught onto it a little bit. She actually even bought me one. I don’t know what that says, but I get in one at least twice a week,” Tuberville said.
“Now, I can’t tell you whether it’s helped me or not, but I do know that we hear from quite a few people that do it on their own that it’s helped so hopefully in the future we can—we can bypass some of the red tape and at least try it—some therapies that are not working on some veterans, hopefully it can help in that area,” the senator added.
Tuberville also claimed 12,000 veterans have received HBOT treatment for TBI or PTSD “with near universal improvement,” while citing that depression scores were reduced by at least 39 percent.
“Anything that is helping folks I agree is a good thing, but before I commit resources and put a lot of energy and emphasis into things at the system wide level, I need to see more convincing and rigorous scientific data,” Wiechers replied to Tuberville’s, also saying that she would like to see the studies backing that statistic.
Panelist and University of Alabama at Birmingham adjunct assistant clinal professor Dr. Jim Wright, meanwhile, spoke in favor of HBOT treatment for TBI and PTSD.
“In treating TBI and PTSD, hyperbaric oxygen has had remarkable results over the last 20 years. It is universally effective,” Wright said. “Few, if any, recipients fail to improve, and many are made completely well from debilitating injuries. Brain function and cognition is improved even after decades of TBI or PTSD.”
Wright also argued that HBOT shows promise in ending suicidal ideation, improving quality of life and reducing medication requirements and chronic pain for veterans.
“I propose that hyperbaric oxygen treatment be made immediately available to our veterans with TBI, PTSD and spinal cord injuries,” Wright said. “The huge quantities of case reports as well as numerous randomized controlled studies speak to the utility and safety of the treatment as well as providing more than enough evidence of efficacy for approval as part of the standard of care.”
Wright also proposed establishing a working group to “design the implementation” of HBOT treatment for veterans, as well as calling for the VA to take immediate action to expand access to potential therapies.
“We need immediate action. Not platitudes, words or more studies on some of these. Some are ready to go like hyperbaric oxygen and probably some of the other treatments,” Wright said.
Wright went on to criticize the VA’s research methodology in its study on hyperbaric oxygen treatments.
“Everybody gets it to work except the VA and DOD,” Wright claimed.
Compass Pathways Chief Patient Officer Dr. Steve Levine spoke regarding his organization’s work to expand access to emerging mental health treatments for veterans, such as their ongoing FDA-regulated clinical trial on the safety and efficacy of psilocybin treatments, which Wright said was the largest in U.S. history.
“The setting is really important and being adequately prepared and the safety setting around you being there is critically important, and that is how these medicines are being studied,” Levine said of psilocybin’s utility in treating PTSD and TBI. “That’s how they will likely be approved and that’s where we see the best outcomes.”
“People may not realize how close we are getting actually to potentially having FDA approvals here,” he added.
Veteran Mental Health Leadership Coalition Director of Operations Adam Marr spoke on he and his family’s experiences discovering alternative pathways to treating PTSD and TBI after their time in the armed forces.
“My older brother Andrew, an SF Green Beret, came home with TBI and PTSD. The system’s answer? Thirteen symptom masking medications and they told him this is your new normal,” Marr said. “Veterans aren’t broken, though. Parts of the system are. For decades care has numbed instead of healed. Pills, brief therapy sessions and labels that never address the root cause of trauma.”
Marr went on to describe the therapeutic benefits the psychedelic drug ibogaine had for his recovery from PTSD ad TBI.
“My own journey with ibogaine became one of the single most transformative experiences of my entire life,” Marr said. “These treatments do, however, carry risks and require medical oversight. For us, though, for my brothers, for my family; they were lifesaving.”
Marr called for further funding to expand research and access to therapies such as psychedelics.
“We must invest in research, expand access and do so expeditiously,” he said, emphasizing the need for “multiple structured settings” when receiving psychedelic therapy for PTSD or TBI in a controlled environment.
“These therapies are producing better and lasting outcomes because they’re able to go to the root cause as opposed to masking the symptoms,” Marr added.
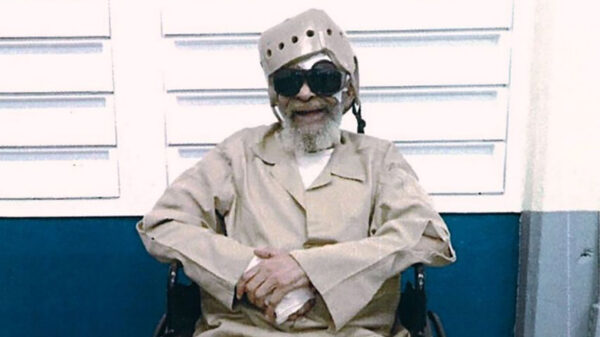
U.S. Air Force veteran and founder of the nonprofit SCI-DI Brian Schiefer also shared his experiences recovering using alternative therapies after a Humvee rollover accident resulting in severe spinal, skull and nerve injuries left him with a TBI, partial paralysis and one working eye.
“It is my testimony that, had I relied only on the standards in care within the VA, I would not be here today,” Schiefer said.
“VA’s care, even for basic needs like wheelchairs, seating cushions, catheters, hand controls has been problematic at best,” he added. “Procurement often required me to navigate, essentially alone, bureaucratic hurdles for essential prosthetic devices and general medical care.”
Schiefer spoke on his experience receiving hyperbaric oxygen therapy following his injuries.
“I experienced immediate improvement in cognition sleep, memory and relationships and no longer waking up in a fog,” Schiefer said.
“I continue to advocate and push for innovative approaches to ensure no one has to endure the hardships and miseries I’ve faced, pressing for systematic changes to make the VA care more responsive and effective for veterans with complex injuries,” Schiefer said of his nonprofit, which helps connect veterans with alternative therapies for mental and physical rehabilitation.
Schiefer went on to describe his experiences with scuba diving and psychedelics as important parts of his recovery.
“Underwater is a barrier-free 3D environment I found liberation in, reduced pain, better sleep and a relief from TBI related cognitive fog, much like HBOT, but with the freedom of floating and movement,” he said.
Schiefer went on to advocate for veterans taking their care into their own hands to overcome what he sees as bureaucratic hurdles.
“I’ve had folks that have gone down to Mexico to receive the ibogaine treatment and were told from their VA provider they were going to lose their benefits if they went” Schiefer said. “These were folks that were taking two shoe boxes full of medications, came back and they were taking none.”
“I think everybody has a need, and if the needs aren’t being addressed here in the states, I would encourage them to go find what works best for them,” Schiefer said when asked by Tuberville for his advice to veterans unable to receive alternative therapies in the U.S.
Ahead of the forum, Tuberville drew criticism from Smart Approaches to Marijuana, a nonprofit that advocates against cannabis commercialization and legalization, and conservative NGO Eagle Forum of Alabama.
In a written statement, U.S. Air Force veteran Rex F. Chilton and U.S. Army veteran Benjamin Scott Jones criticized Tuberville for platforming researchers and advocates connected with psychedelic treatments for veterans.
“As veterans and residents of Alabama, we are disappointed that Senator Tuberville is giving airtime to drug legalization advocates and people biased by profit in a hearing on treatments for veterans’ PTSD,” they wrote. “We need community, connection, and proven non-drug solutions that work. Not the latest unproven drug cocktails being rushed forward for the sake of profit over veteran lives and well-being.”
“We are confident that Senator Tuberville and other committee members will take great caution to avoid risky and unproven therapies and balance their views with the full spectrum of serious, evidenced based patient care,” wrote Eagle Forum of Alabama medical advisor Christine C. Carr. “Our medical experts strongly advise against the use of potentially deadly and poorly managed substances which may preemptively further the commercialization of these drugs.”