By Bill Britt
Alabama Political Reporter
MONTGOMERY—Speaker Mike Hubbard cast repeated votes in favor of House versions of a bill giving exclusive rights to manage Alabama’s Medicaid prescription drug purchasing to a company that employs Hubbard under a lucrative public relations contract.
In a series of eleven YES votes cast on April 23rd on state House versions of the General Fund budget, Hubbard actively sought to ensure his public relations client – American Pharmacy Cooperative Inc. – became the sole company eligible to provide Pharmacy Benefits Manager services to Alabama’s Medicaid agency.
Though he voted multiple times in favor of the legislation, Hubbard never publicly disclosed his financial ties to American Pharmacy Cooperative Inc. (APCI), the company that stood to profit from Medicaid provisions of the budget. Nor did Hubbard declare a conflict of interest or abstain from taking official action on the bill, titled SB143.
While the details of Hubbard’s contract with APCI are unknown, Hubbard’s official actions favoring APCI appear to violate state ethics laws regarding conflicts of interest.
According to the Alabama Revised Ethics Code, “(A) conflict of interest involves any action, inaction, or decision by a public official or public employee in the discharge of his or her official duties which would materially affect his or her financial interest or those of his or her family members or any business with which he person is associated in a manner different from the manner it affects other members of the class to which he or she belongs.”
The provisions of the bill Hubbard voted on contained language that, if implemented, would have meant anywhere from $12 million to more than $20 million for his client, according to estimates of state finance experts.
State Ethics Commission Director James L. Sumner and American Pharmacy Cooperative Inc. CEO Tim Hamrick confirmed last week that Speaker Hubbard has an financial agreement with the company to promote “membership growth strategies” in 23 states around the country.
Hubbard’s repeated votes on the House versions of the 2014 General Fund budget came as the Gov. Bentley administration strongly objected to adding the pharmacy language which several officials said was designed to exclusively benefit APCI.
“Yeah, I understood that it would only benefit one particular group, based on the language that was put in there,” said state Rep. Steve Clouse, vice chairman of the House Ways and Means General Fund Committee, and sponsor of the House version of the General Fund budget bill.
State Health Officer Don Williamson had a similar understanding. “It was my understanding that there was only one company in Alabama that would meet that criteria.” Asked if that company was APCI, Williamson said, “Yes, sir, that was my understanding.”
The General Fund budget is typically complicated legislation, going through a number of variations before final passage. This year was no different.
SB143 was originally drafted by Sen. Arthur Orr, Republican chairman of the Senate Finance and Taxation General Fund Committee. The bill was introduced in February and finally passed out of the Senate with three amendments on March 12th. When state Senators sent the budget to the House, there was no language benefitting APCI. But by Feb. 23rd, the House had re-crafted the budget adding a section that would have forced the state into using a Pharmacy Benefits Manager to administer the Medicaid prescription drug purchased.
According to the bill:
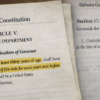
“The Alabama Medicaid Agency, in order to implement a pharmacy benefit manager program, must seek a pharmacy benefit management organization or manager that will: (i) act in fiduciary capacity and perform its duties in accordance with standards of conduct applicable to a fiduciary, including the allocation of all drug manufacturer rebates, discounts, and incentives to the State General Fund; (ii) establish a maximum allowable cost list; and (iii) operate a group purchasing function with a purchasing base for generic drugs consisting of at least 30% of the retail pharmacies in Alabama.“
Those 23 words requiring the PBM have a purchasing base of 30 percent locked in Hubbard’s client, APCI, as it is the only company that fits the description, officials said.
Asked if Hubbard pushed for the PBM language to be added to the bill, Rep. Clouse said he did not recall. “You know we (Clouse and Hubbard) talk about a lot of things with the budget. I don’t remember in particular.” Clouse said he recalled Rep. Greg Wren suggested the passage benefiting APCI. Wren was “concerned about independent pharmacists and he wanted to add language in there… Greg wanted to put the language in there, so I told him to go ahead and write it up.”
Neither Hubbard or Wren responded to multiple phone messages and emails seeking comment for this story.
Calls were also made to G. Ferrell Patrick, APCI’s lobbyist in Montgomery. Patrick did not return the Alabama Political Reporter’s calls for comment.
Williamson, the state Health Officer, said he grew increasingly concerned that the PBM provisions limited the state’s ability to find an appropriate PBM. Indeed, the state’s options were limited to a single company – Hubbard’s client. Williamson, as the governor’s point-man on Medicaid worked until the last days of the session to find a compromise to the language inserted into the House budget.
Sen. Orr said that just days before the end of session, “This was one of the last things hanging out there that was not going to work for [Medicaid]. Williamson, got engaged and worked diligently for what I call compromise language…that would leave him with flexibility to issue a RFP [Request for Proposal] for PBMs effective next year. Williamson categorized the negotiations as tough and confrontational.
The Governor has since signed and executive order establishing the Alabama Medicaid Pharmacy Commission. The commission is tasked with comparing Alabama’s handling of Medicaid pharmaceutical benefits with programs in other states and will study options to reduce Alabama Medicaid’s pharmacy costs while still maintaining a quality Medicaid program, according to the order.
Williamson said that Medicaid needed to understand how each PBM worked so that they could negotiate what would be in the best interest of Alabama.
According to Dennis L. Tumminia, Senior Employee Benefits Consultant Edgewood Partners Insurance Center, “PBM’s typically employ a “balloon strategy” in their price negotiations – if you squeeze one element of the pricing matrix another element inevitably “pops” out somewhere else. Ask for a lower administrative fee, for example, and the dispensing fee becomes non-negotiable. Ask for a lower ingredient cost discount and rebates begin to disappear.”
Tumminia says that it is important for those seeking contract a PBM understand that, “PBM’s utilize a “per script” net revenue model that combines all of the revenue elements. So, if you are going to be successful in your negotiations, you need to understand what those specific revenue elements are. Some PBM revenue elements, like administrative fees, are highly visible. Others, like rebates, are shrouded in confidentiality agreements.”
Williamson said that the language inserted in the House — language favoring Hubbard’s client—was the biggest problem with the bill. It “was the issue we had concerns about, if there were others [problems with the bill] I didn’t know about them.”